The Ffect of Music Gtherapy for Patients With Huntingtons Disease a Systematic Literature Review
- Study protocol
- Open Access
- Published:
Music therapy in Huntington'southward disease: a protocol for a multi-centre randomized controlled trial
BMC Psychology book 4, Article number:38 (2016) Cite this article
Abstract
Background
Huntington's illness is a progressive, neurodegenerative disease with autosomal dominant inheritance, characterized past motor disturbances, cognitive decline and behavioral and psychological symptoms. Since there is no cure, all treatment is aimed at improving quality of life. Music therapy is a non-pharmacological intervention, aiming to amend the quality of life, just its utilize and efficacy in patients with Huntington'southward disease has hardly been studied.
In this commodity, a protocol is described to study the effects of music therapy in comparing with a command intervention to improve quality of life through stimulating expressive and chatty skills. By targeting these skills we assume that the social-cognitive functioning will improve, leading to a reduction in behavioral bug, resulting in an overall improvement of the quality of life in patients with Huntington'due south disease.
Methods/Pattern
The study is designed as a multi-middle single-blind randomised controlled intervention trial. Sixty patients will be randomised using eye-stratified cake-permuted randomisation. Patients will exist recruited from 4 long-term care facilities specialized in Huntington's disease-care in The netherlands.
The outcome measure to assess changes in expressive and communication skills is the Behaviour Observation Scale Huntington and changes in beliefs will be assessed past the Problem Behaviour Assesment-short version and by the BOSH. Measurements accept identify at baseline, then 8, 16 (end of intervention) and 12 weeks after the terminal intervention (follow-up).
Give-and-take
This randomized controlled study will provide greater insight into the effectiveness of music therapy on activities of daily living, social-cognitive performance and beliefs problems by improving expressive and communication skills, thus leading to a better quality of life for patients with Huntington's disease.
Trial registration
Netherlands Trial Register: NTR4904, registration engagement Nov. 15, 2014.
Background
Huntington'due south Disease (Hard disk drive) is a progressive, neurodegenerative disease with autosomal dominant inheritance, caused by an elongated CAG echo on chromosome 4 [ane]. HD is characterized by motor disturbances, cognitive decline and behavioral and psychosocial symptoms. The cerebral disorder in Hard disk drive effects a wide variety of skills, including learning and memory, perceptual skills, executive efficiency and language [ii]. Cognitive and behavioral changes are the near debilitating aspects of the affliction and place the greatest burden on the patient as well equally on their families and caregivers, and are ofttimes the main reason for institutionalization [iii, 4]. Affective (mood) disorders (e.g. depression, feet, apathy, irritability) and behavioral problems (e.g. obsessive compulsive beliefs and assailment) are frequent symptoms [5].
Verbal communication is often affected, due to motor impairment of speech. In improver, as a result of the cognitive decline, give-and-take retrieval is ofttimes dumb, although the knowledge of vocabulary is retained. Equally the disease progresses, the linguistic communication content can no longer be processed properly and in the later on stages of the disease, a patient with HD might not be able to communicate adequately [1].
Equally a outcome of the communication problems, patients are no longer able to express themselves. Revealing the patients' unmet needs is, therefore, hindered and this might pb to irritability, impulsive and unwanted beliefs (frequently signs in HD), causing much distress for patients and caregivers. Because of the behavioral symptoms, cognitive decline and the inability to express oneself, psychosocial problems develop [6]. Psychosocial stressors may include feelings of sadness and feet about the cognitive and concrete reject, and about changes in social roles [seven]. The gradual deterioration in communication skills, in combination with the behavioral issues in patients with Hard disk, contributes to a subtract of functional health and a progressive inability to participate in various life situations, leading to loss of quality of life [8].
Since at that place is no cure for Hd, the aim of all therapy, both pharmacological and non-pharmacological, is to meliorate quality of life [9]. 1 grade of non-pharmacological intervention is music therapy.
Music therapy uses music experiences and patient-therapist relationships in lodge to effect therapeutic modify [10]. Over the past decades, music therapy has been developed for patients with neurodegenerative diseases [11, 12]; its efficacy is shown in Table 1.
There is evidence that music therapy influences emotional well-being positively and that participation in music therapy increases social response in people with dementia [13]. It can decrease agitation and has a positive effect on enhancing communication and emotional well-beingness. Music therapy enables the recall of life experiences and the feel of pleasant emotions. Through music, contact tin be established, especially as linguistic communication deteriorates during the later stage of the dementing process [14, 15].
In a comprehensive literature search, Lee and McFerran [16] conclude that the non-verbal communication skills in individuals with profound and multiple disabilities meliorate as a issue of song-pick during music therapy sessions. The results of their written report support the conventionalities that, through music therapy, the power to express oneself will improve, contributing to comeback in the quality of life.
Furthermore, in a literature review, Patel et al. [17] demonstrate the effectiveness of MT in reducing behavioral and psychological symptoms of dementia. Several other meta-analyses and literature reviews have concluded that music therapy decreases symptoms related to behavioral problems in dementia [eighteen–twenty].
On the basis of the above-mentioned literature, the assumption can be made that music therapy might be beneficial to patients with HD. Although knowledge on the use and efficacy of music therapy in Hard disk drive is limited, it has been suggested that it can improve the communication skills of people with HD [21]. Past improving the expressive and communication skills through music therapy (which volition be assessed by the BOSH) we hypothesize that behavioral problems will decrease (assessed by the BOSH and the PBA-s), leading to an overall improvement of quality of life.
To test this hypothesis, we wrote a report protocol to reply the following questions:
- 1.
Does music therapy ameliorate expressive and communicative skills in people with Hd?
- two.
Does music therapy reduce behavioral problems in patients with HD?
- 3.
Does music therapy amend the quality of life of patients with HD?
Methods
Study design
The report is a multi-centre, unmarried-blind, randomised controlled intervention trial with 2 parallel arms. An overview of the study blueprint is shown in a flow chart (see Fig. 1). Information technology is single-blinded; the researcher who analyses all the scores is unaware of the allocation of the patients throughout the report. Too, the persons performing the baseline-assessments will be kept unaware of the allocation of the participants they are testing. Threescore patients (come across sample size calculation below) volition be randomised using centre-stratified, block-permuted randomisation post-obit the procedure every bit described beneath. 2 random groups volition be created. The experimental group will be offered a music therapy program according to a structured protocol (see below), and the control group volition participate in recreational 24-hour interval activities, following the same protocol as the experimental group. In add-on, both groups will receive regular treatment (standard care, treatment equally usual). Participants from both the experimental and the control groups volition not be allowed to receive music therapy outside the study.
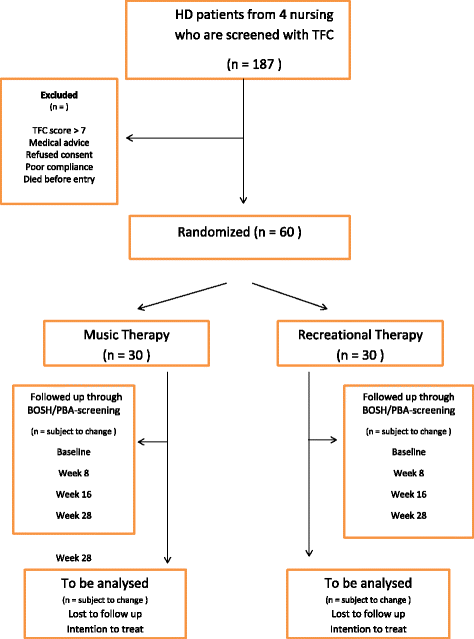
Flowchart
Procedure
Recruitment
Patients will be recruited from four long-term care facilities (nursing homes) in Kingdom of the netherlands, all specialized in HD, with 1 or more units exclusively for Hd-patients. Recruitment will be primarily done by the nursing staff and the responsible medico.
Inclusion and exclusion criteria
Eligible patients must meet the following inclusion criteria:
-
Historic period older than xviii years
-
Clinically and genetically confirmed Huntington's Disease (CAG ≥ 36 repeats)
-
Total Functional Capacity (TFC) ≤7
Exclusion criteria:
-
patients who suffer from other neurological disorders
-
patients with poor comprehension of the Dutch language
-
patients who have received music therapy in the past three months
-
patients with a hearing damage
Patients will be included irrespective of medication condition and volition be allowed to continue medication during the report. However, any change in medication should exist avoided and carefully registered.
Informed consent
Informed consent will be obtained by the nursing staff from patients who are cognitively able to understand the possible risks and benefits of the study. Proxy consent will be obtained from next of kin, or a legal guardian, if the patient is non able to give an informed consent.
Baseline assessments
Clinical and demographic variables such every bit gender, age, (changes in) medication, number of CAG-repeats and (estimated) age at onset volition be gathered for each participant. The stage of Huntington'south Illness volition be assessed using the Total Functional Capacity (TFC) [22]. The TFC, role of the Unified Huntington Affliction Rating Scale, consists of 13 points and contains 5 domains: work, finances, domestic chores, activities of daily living and care requirements [22]. Every bit the illness progresses, the TFC-score will drib, giving clinicians a good indication about the functional phase of the affliction. A score of vii or lower indicates that the patient is in the mid/advanced stage, and so impaired in his functional capacities that assistance with self-care is needed [22]. Most of the patients that reside in the four long term care facilities that participate in the written report have a TFC-score of 7 or lower. To ensure a homogeneous group, patients with a TFC score of > seven will be excluded from participating in the research The TFC will be administered by the elderly intendance physician who is responsible for the patient.
The Mini Mental Land Test (MMSE) will be used to assess the cerebral function of the patients at baseline. A score of 23 or lower out of 30 indicates cognitive impairment [23]. The MMSE will be administered by the psychologist or the psychology assistant.
Randomisation
In order to minimize the impact of any betwixt-center differences on the trial results, the participating centers volition exist stratified in the randomization process. Participants will be randomly assigned to either command or experimental grouping with a 1:ane resource allotment. To generate the random allocation sequence we apply the method of center-stratified, cake-permuted randomization [24]. The cake size will vary. To diminish the risk of predictability, the date of signing the informed consent volition determine the sequence in which the patients will be randomized. Non until all baseline measurements have been completed, the randomization code will exist released to ensure allocation darkening.
Randomization will be conducted without any influence of the principal investigators, raters or therapists.
Intervention
All participants (in both the experimental (intervention) group and the control grouping) volition continue to receive handling every bit usual. The intervention grouping will receive music therapy (MT-group). The control group will receive recreational therapy. The number of sessions (16) is equal in both groups, as are the 24-hour interval of the calendar week and the time of the day at which the sessions will take place. Patients in both groups will participate in grouping interventions with 3 to v participants.
It must be noted that each of the iv participating facilities have a different music therapist and recreational therapist attached to the research. However, all participating therapist accept been instructed thoroughly to follow the same protocol. The reports that the therapist will fill up out afterwards each session will exist used to monitor whether they have followed the instructions. Come across "compliance with treatment".
Intervention grouping
The music therapists committed to the written report are professionally trained and take been specifically informed about the clinical method and its theoretical footing.
The principal goal of the music therapy intervention is to heighten advice skills past mode of encouraging and stimulating the patients in interaction. The music therapy arroyo applied in this written report is focused on encouraging and engaging patients in expressive musical interaction. The office of the therapist is to use musical parameters and interventions to stimulate expressive and chatty skills. The caste of verbal reflection may vary; the therapist volition, nonetheless, encourage the participants to limited themselves. The therapeutic process is based on the mutual construction of significant of emerging thoughts, images, emotional content and expressive qualities that often originate from the musical experience [10].
A treatment guide specifies the procedures. It outlines the setting, goals and basic principles of the intervention; Table 1 (the benefits of music therapy for neurodegenerative diseases) is used as guideline. The available music therapy techniques to target the set goals are derived from the protocol "music therapy for Huntington's patients on improving and stimulating communication and self-expression" [25]. Notwithstanding, the guidelines are to be administered flexibly according to the patient's state of mind and his needs at that very moment. The clinical expertise of the therapist will be the guide, providing the therapist with enough "space" for flexible adaptation within the treatment guide. As well, the patients music preference, particularly because most of the treatment involves receptive music therapy, is very of import. This is the reason why the protocol allows and encourages the music therapist to adjust their treatment by way of "tailor made" sessions, providing each of the participants with his or her music preference.
The process used in each session is standard while the content is flexible. The intervention will be provided at the same time of the same mean solar day of the week by a formally trained, experienced music therapist. The sessions will take identify once weekly with a total of 16 sessions, lasting 45 min. They will be standardized without limiting the music therapists in their interactions. The intervention itself, nonetheless, volition exist (partly) applied co-ordinate to a protocol. Each session starts with the same welcome song/musical piece and ends with the same farewell song/musical piece. In doing so, the participants become familiar with the showtime and the terminate of each session. In betwixt these 2 songs/musical pieces, the music therapist adjusts the level of each intervention to individual capacities. After the welcome song, the music therapy sessions may be varied: the music experiences can range from listening to music to playing or singing songs to gratis improvisation. therapist has the freedom to determine what works all-time at that very moment for that specific patient. The participants will listen to music selected, sung or played by the therapist. Active participation in music activities by singing or playing a musical musical instrument will exist stimulated as much as possible. The music will be selected by the music therapist to incite expressive and advice skills and to reduce agitation, based on musical parameters, such every bit rhythm, melody, harmony, dynamics, timbre. Later on each vocal/musical intervention, the therapist will encourage and stimulate the participants to reflect verbally on the music [25].
Besides the music therapy intervention during the whole study, participants are not allowed to receive additional private music therapy.
All participants are allowed to leave the session at all times.
Control grouping
All activities will be provided by professionally trained recreational therapists who have been specifically informed well-nigh the study.
In the command group, recreational day activities will be offered under exactly the same circumstances as the music therapy sessions: a total of 16 weekly sessions, each lasting 45 min, every calendar week at exactly the same time as the music therapy intervention. Equally in the intervention group, a treatment guide specifies the treatment procedures for the control grouping. In this guide, the setting and general goals are outlined. The main goal of the recreational activities is to enhance communication skills by style of encouraging and stimulating the patients in interaction.
The activities vary from reading the newspaper, cooking, arts-and-crafts/handwork or puzzles/games. Musical activities, such as singing along or watching a music-video are non allowed, nor will background-music be played. The recreational therapist is well instructed about and fully aware of this brake. Besides that, during the whole study, participants from the control group are not allowed to receive music therapy. Both the doc who is responsible for the referrals and the music therapists are fully enlightened of this limitation. Participation in in regular musical activities withal (such as watching a music video or attending a music-performance which takes place on the ward occasionally) is immune. These activities are not considered to be music therapy and are open to all patients that reside in the institution, regardless of participation in the study. Also, listening to music in the privacy of their ain room is allowed for all participants.
All participants are allowed to exit the session at all times.
The music therapy and the recreational day activities will be provided in separate rooms, away from the ward. Participants will be taken to the music therapy room or the activity room by the nursing staff. The music therapist and the recreational therapist make certain that they can outset the moment all participants are in the room. Afterwards the session, the participants will be taken dorsum to the ward by the nursing staff. The therapists will never go out a participant in the room unattended.
Later on each session, a short written report of the activities volition be written by both therapists, including an evaluation of each patient. Since a self-report from the patient himself is not feasible, the reports written by the therapists volition be used for evaluation purposes and handling fidelity.
Compliance with handling
In each participating center a monitor will be identified, to be responsible for adherence to study protocol (including data collection).
Furthermore, after each session, both therapists will document significant events, notable behaviors, and interventions applied. These reports will enable u.s. to determine whether the handling has been conducted as intended. These reports will provide insight into the patient'southward state of mind at the time of the intervention. This information tin help us explicate why certain measurements might be significantly different compared to others in the same patient. Cocky-reports (the patients' own perception) might not be viable, due to the rapid decline of cognitive skills (run across rationale), Furthermore, this data will also be used to evaluate the process of the report.
Outcome measures
The main outcome measure, advice skills, will exist assessed past the social-cognitive domain of the Behaviour Observation Scale Huntington (BOSH) [26]. The secondary outcome measure, behavior, will be assessed by both the Trouble Behaviours Assessment-curt version [27, 28] and the third domain (mental rigidity and assailment) of the BOSH (mental rigidity and aggression).
The BOSH contains 32 items in three subscales: 1) activities of daily living (ADL) (five items), 2) social-cognitive functioning (15 items), and iii) mental rigidity and aggression (12 items). Each item is assessed on a iv-indicate scale. The scores from the showtime subscale (ADL) range from i (self-supporting) to 4 (nursing required). The sum score from the outset scale may range from 5 to xx. The scores from the second subscale (social-cerebral functioning) range from 1 (unaffected) to four (contact no longer possible); the sum score may range from fifteen to 60. Finally, the scores from the third subscale (mental rigidity and aggression) range from one (never) to 4 (always); the sum score may range from 12 to 48. Intra- and interrater reliabilities are respectively 0.83 and 0.95 [26].
Assessment of the BOSH will take place within a week before the outset intervention (baseline assessment), and will be repeated within a week later on the 8th and again within a week afterwards the 16th intervention. 12 weeks after the final intervention, the BOSH volition exist repeated.
The BOSH takes fifteen min and will exist administered past nursing staff in charge of the daily care of the patients. Blinding the BOSH-assessors might non be viable as the nursing staff will take to send the patients to and from the therapy-rooms. Also in daily life, the chance of the patient divulging his or her allocation towards the nursing staff is big. Even so, in the process-evaluation following the report all the assessors will exist asked whether they were aware of the allocation of the patients.
Since the BOSH is a commonly known assessment calibration in the participating Hard disk nursing homes in Holland, no formal training will be carried out prior to the offset of the study unless the detail nursing dwelling has no experience with the BOSH.
Behavioral problems will be assessed with the Problem Behaviours Cess-curt (PBA-s) version [27, 28]. This is a 5-point rating calibration, using the scores 0 (absent-minded) to 4 (severe). The PBA-s is a 11-item semi-structured interview and assesses behavioural problems in the 4 weeks prior to the interview. The sum score may range from 0 to 40. In add-on, there is a subscale for severity and one for frequency. The PBA-southward is a validated and reliable measurement-tool: the interrater reliability is 0.74 for severity and 0.76 for frequency scores (mean kappa), and 0.94 for severity and 0.92 for frequency scores (weighted kappa) [29]. The respondents of this face to face semi-structured interview are the patient and a knowledgeable informant (spouse or caregiver) together.
Cess of the PBA-s will have place following the same time-schedule as the BOSH-assessments. The PBA-s will be scored by independent, formerly trained assessors who will be blinded to group allocation of the patients. Later the terminal assessment, the assessor volition be asked whether or non he inadvertently institute out about the patient'southward resource allotment in social club to verify the success of the blinding. Where possible, subjects are interviewed in the presence of a knowledgeable informant (chief caregiver).
After consulting a member of the PBA-workgroup we decided to arrange the 4-week retrospective view of the PBA-s to ane week, due to the short time-frame in which it is administered (every eight weeks).
Sample size
The minimal clinically important change or divergence (MCIC/MCID) in the scale serves equally important input for the sample size calculations. Unfortunately, data nigh these calibration-characteristics are unavailable. We conceptualize that the population in the present report volition differ little from the population previously used in the study by Timman et al. [26] from which we derived data on means and standard deviations for the subscales of the BOSH. If we presume that the values in the control group will alter footling over the course of the study, whereas those in the experimental group will improve by 25 %, and if we further presume an α of 0.05 and a β of 0.20, and then the post-obit sample size would be required:
-
ADL: original mean ± SD = 2.25 ± 0.88; improvement of 25 % volition effect in a hateful of 1.69 and if nosotros conservatively estimate a reduction in SD to 0.75, we would crave an Northward of 30 per group for the ADL subscale (for an effect size of 0.55 (moderate));
-
Social-Cognitive: original hateful ± SD = 2.10 ± 0.79; improvement of 25 % volition result in a hateful of 1.58 and if we conservatively estimate a reduction in SD to 0.75, we would likewise require an N of 30 per grouping for this subscale (for an upshot size of 0.52 (moderate)).
Data management and confidentiality
Participant files volition exist stored in locked cabinets with limited access. Participating centers will only accept access to their ain center's information. Data will exist entered into SPSS by an independent inquiry assistant. Afterward the trial the main investigators and the statistician volition have access to the data set.
Statistical analysis
The primary outcome measures of this study are the differences in total and subscale-scores of the ADL and Social-Cerebral subscales of the BOSH and the PBA-s between groups (command versus MT) when baseline differences are taken into account.
Results will be analyzed on an intention-to-treat basis.
A mixed model analysis with repeated measures will be used to analyze the differential effects of music therapy versus recreational activities on the four GOSH and PBA-due south scores (week 0, week 8 and week sixteen, and a follow-up score in calendar week 28). The assessment number, ranging from i to four, will exist used as the fourth dimension variable of the repeated measures.
As stratified randomization frequently leads to correlation between treatment artillery, it is necessary to adjust for the stratification factors in the analysis to obtain correct confidence intervals and p-values. By doing so, we maintain the type I error rate at its nominal level (usually set at v %), and avoid a reduction in ability [30].
Discussion
Music therapy is a promising non-pharmacological intervention. Through stimulation of the expressive and communicative skills, it is hypothesized that this therapy will result in improving activities of daily life and social-cerebral functioning likewise every bit reducing behavioral problems, thus leading to an improvement in the quality of life.
In general, music therapy tin be offered either individually or in grouping sessions, with other patients or with family unit members. The sessions tin can be "tailor-fabricated" for the patient and his needs.
In this study, patients in both the intervention- and the command group volition participate in grouping interventions with three to five participants. The decision to choose group-interventions rather than individual interventions is based on the assumption that the interaction between grouping-members will stimulate communication [31]. In this article, Magee concludes that music therapy is recommended in the middle and the advanced stages of HD. Group sessions allow the patient the fourth dimension needed for delayed responses, assuasive natural "time out" from responses which require attending or concentration. The number of participants in each grouping has to be determined carefully. In a systematic literature review, Ing-Randolph et al. [32] propose that group size matters with music interventions addressing certain stages of dementia-associated anxiety. Although Yalom [33] states that a group consisting of fewer than five members results in a decrease in member interaction, this is not the case when working with HD-patients where smaller groups are preferable [31].
Based on earlier RCTs and a meta-assay of the dose-issue relationship of music therapy in unlike settings and populations, we expect a treatment duration of 16 weekly sessions, each session lasting 60 min, to be sufficient for detectable developments [13, 14].
The determination to employ the BOSH every bit the primary outcome measures instead of a QoL-scale requires some clarification; in our opinion, no validated QoL-scale (generic nor affliction-specific) is sufficiently sensitive to be used in the very late phase of the disease.
The BOSH was developed to provide an observational instrument for monitoring the behavioural aspects of the patient in later stages. Expressive and communicative skills are specifically measured within the social-cerebral functioning-subscale. In combination with its ii other subscales (ADL and mental rigidity), we believe that the calibration is so broad that it covers most of the QoL-domains. In the nowadays report, nosotros are planning to clarify the total score of the BOSH.
Conclusion
This commodity outlines the study protocol of a randomized controlled trial providing insight into the effects of a structured group music therapy intervention for patients with Huntington's disease. More specifically, the furnishings of music therapy on improving quality of life through specifically targeting the expressive and chatty skills, in comparing with an active control intervention, will be tested.
Conclusions that volition sally from this study are expected to contribute to evidence-based handling for Huntington's Disease patients who experience deterioration of expressive and communicative skills, leading to a reduction in behaviour problems, and resulting in an overall improvement in quality of life.
Nature and extent of the brunt and risks associated with participation, benefit and grouping relatedness
It is non expected that the intervention will be a serious burden for or risk to the participants, nor are physical or physiological discomforts associated with this study.
Reporting of study results
The study results will be disseminated in the post-obit ways:
-
A last report
-
Formal publications in peer reviewed high bear upon international periodical
-
Presentations in dissimilar international conferences
-
Dissertation and public defense
Protocol amendments
Any modifications to or authoritative changes or clarifications of the protocol that have no outcome on the way the study is to exist conducted volition be reported to the Dutch Trial Register (NTR 4904).
Abbreviations
BOSH, Behavioural Ascertainment Calibration for Huntington; Hard disk, Huntington's illness; LTCF, long term care facility; PBA-southward, Trouble Behaviour Cess-curt version; QoL, quality of life
References
-
Bates G, Harper PS, Jones Fifty. Huntington's disease. Oxford: University Press; 2002.
-
Nance Chiliad, Paulsen JS, Rosenblatt A, Wheelock V. A Doc's guide to the management of Huntington's Affliction. Huntington's Disease Society of America, third edition 2011.
-
Roos RAC. Huntington's affliction: a clinical review. Orphanet J Rare Dis. 2010;five:twoscore.
-
Hamilton JM, Salmon DP, Corey-Blossom J, Gamst A, Paulsen JS, Jerkins S, Jacobson MW, Peavy G. Behavioural abnormalities contribute to functional decline in Huntington's disease. J Neurol Neurosurg Psychiatry. 2003;seven four(1):120–2.
-
van Duijn E, Kingma EM, vander Mast RC. Psychopathology in verified Huntington's illness cistron carriers. J Neuropsychiatry Clin Neurosci. 2007;19:441–8.
-
Vervoort Eastward, van FJ Z. De ziekte van Huntington en verwante erfelijke neuropshiatrische aandoeningen. Assen: Van Gorcum; 2009.
-
A'Campo LEI. A patient and caregiver eduction program in Parkinson'south illness, Huntington's disease, and other chronic diseases. PhD-thesis, Leiden Academy Medical Centre, Leiden 2012. Chapter 7: 115–131. ISBN: 978-90-5335-542-viii.
-
Ho AK, Robbins AOG, Walters DJ, Kaptoge Due south, Sahakian BJ, Barker RA. Health-related quality of life in Huntington'due south affliction: a comparison of two generic instruments, SF-36 and SIP. Mov Disord. 2004;nineteen(xi):1341–eight.
-
Thaut MH, Miltner R, Lange HW, Injure CP, Hoemberg V. Velocity modulation and rhythmic synchronization of gait in Huntington'southward illness. Mov Disord. 1999;14(v):808–nineteen.
-
Erkkilä J, Gold C, Fachner J, Ala-Ruona E, Punkanen M, Vanhala M. The upshot of improvisational music therapy on the handling of low: protocol for a randomised controlled trial. BMC Psychiatry. 2008;eight:50.
-
Cohen-Mansfield J. Use of patient characteristics to determine non-pharmacologic interventions for behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2000;12 Suppl 1:373–eighty.
-
Aldridge D. Music therapy and neurological rehabilitation: performing health. 1st ed. London/Philadelphia: Jessica Kingsley Publishers; 2005.
-
Vink AC, Zuidersma M, Boersma F, de Jonge P, Zuidema SU, Slaets JP. The outcome of music therapy compared with general recreational activities in reducing agitation in people with dementia: a randomised controlled trial. Int J Geriatr Psychiatry. 2013. doi:10.1002/gps.3924.
-
Vink AC. The problem of agitation in the elderly and the potential do good of music. In: Aldridge D, editor. Music therapy and dementia intendance. London: Jessica Kingsley publishers; 2005.
-
Brotons M. An overview of the music therapy literature relating to elderly people. In: Aldridge D, editor. Music therapy and dementia care. London: Jessica Kingsley publishers; 2005.
-
Lee J, McFerran Chiliad. The comeback of non-verbal communication skills of five females with profound and multiple disabilities using song-choices in music therapy. Voices. 2012;12(three). https://voices.no/index.php/voices/article/view/644/559
-
Patel B, Perera 1000, Pendleton J, Richman A, Majumdar B. Psychosocial interventions for dementia: from evidence to do. Adv Psychiatr Treat. 2014;xx:340–nine. doi:ten.1192/apt.bp.113.011957.
-
Vink AC, Bruinsma MS, Scholten RJS. Music therapy for people with dementia (updated Cochrane Review). In: The Cochrane Library. Chichester: Wiley; 2011.
-
Opie J, Rosewarne R, O'Çonnor D. The efficacy of psychosocial approaches to behavioral disorders in dementia: A systematic literature review. Aust Due north Z J Psychiatry. 1999;33:789–99.
-
Sherrat 1000, Thronton A, Hatton C. Music interventions for people with dementia: a review of the literature. Aging Mental Wellness. 2004;8(1):3–12.
-
van Bruggen-Rufi CHM, Roos RAC. The effect of music therapy for patients with Huntington's Disease. a systematic literature review. J Lit Art Stud. 2015;5(1):thirty–forty. doi:10.17265/2159-5836/2015.01.005m.
-
Shoulson I, Fahn South. Huntington's disease: clinical care and evaluation. Neurology. 1979;29:1–3.
-
Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive land of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
-
Ostelo RWJG, Verhagen AP, de HCW V. Onderwijs in wetenschap: lesbrieven voor paramedici. tertiary ed. Houten: Bohn Stafleu van Loghum; 2012.
-
Bruggen-Rufi van CHM. Muziektherapie voor cliënten die lijden aan de ziekte van Huntington ter bevordering en stimulering van communicatie en zelfexpressie ("music therapy for Huntington's patients on improving and stimulating advice and self-expression". Product-omschrijving Trimbos-Instituut. 2009. http://www.vaktherapie.nl/userfiles/files/Producten/2010-07-07_Individuele_MT_voor_clienten_die_lijden_aan_ziekte_Huntington.pdf
-
Timman R, Claus H, Slingerland H, van der Schalk M, Demeulenaere S, Roos RAC, Tibben A. Nature and development of Huntington Disease in a nursing habitation population: the Behavior Ascertainment Scale Huntington (BOSH). Cog Behav Neurol. 2005;18(4):215–22.
-
Craufurd D, Thompson JC, Snowden JS. Behavioral changes in Huntington Affliction. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(4):219–26.
-
Kingma EM, van Duijn Eastward, Timman R, van der Mast RC, Roos RAC. Behavioural problems in Huntington´s affliction using the Problem Behaviours Assessment. Gen Infirmary Psychiatry. 2008;30:155–61.
-
Callaghan J, Stopford C, Arran N, Boisse MF, Coleman A, Santos RD, Dumas EM, Hart EP, Justo D, Owen G, Read J, Say MJ, Dutt A, Leavitt BR, Roos RA, Tabrizi SJ, Bachoud-Levi AC, Bourdet C, van Duijn Eastward, Craufurd D. Reliability and factor construction of the Curt Trouble Behaviours Assessment for Huntington'southward disease (PBA-s) in the Runway-Hard disk and REGISTRY studies. J Neuropsychiatry Clin Neurosci. 2015;27(1):59–64. doi:10.1176/appi.neuropsych.13070169.
-
Kahan BC. Accounting for center-effects in multicentre trials with a binary event – when, why, and how. BMC Med Res Methodol. 2014;14:20. doi:10.1186/q1471-2288-14-20.
-
Magee W. Instance studies in Huntington'south Affliction: music therapy assessment and treatment in the early to advanced stages. Br J Music Ther. 1995;9(two):13–9.
-
Ing-Randolph AR, Phillips LR, Williams AB. Group music interventions for dementia-associated anxiety: A systematic review. Int J Nurs Stud. 2015. doi:ten.1016/j.ijnurstu.2015.06.014.
-
Yalom I. The theory and practice of grouping psychotherapy. New York: Basic Books; 1975. p. 284–vi.
Acknowledgement/Funding
This written report is financed by the Jacques and Gloria Gossweiler Foundation (JGGF), Switzerland. The funding source has no role in the study design and will not accept any role during its execution, analyses, interpretation of the data, writing of the manuscript or in the decision to submit the manuscript for publication.
Availability of data and materials
The consummate datasets that volition be collected and analyzed during the current study are available from the corresponding writer on reasonable request.
Authors' contributions
MB is a clinically trained music therapist. She drafted the manuscript. AV is a psychologist. She reviewed the manuscript. WA is professor of institutional and elderly care medicine and reviewed the manuscript. RR is a neurologist and contributed to the development of the study design and reviewed the manuscript. All authors accept been involved in revising the manuscript, and have read and approved the last text.
Authors' data
MB is neurological music therapist fellow and lecturer at ArtEZ School of Music in Enschede, Kingdom of the netherlands, and researcher at Atlant Care Group in Apeldoorn, Holland.
AV is psychologist and lecturer at ArtEZ School of Music in Enschede, Kingdom of the netherlands, and researcher at KenVak, a research middle for the art therapies in Kingdom of the netherlands.
WA is elderly care physician, specialized in institutional intendance and elderly intendance medicine at the department of public health and primary intendance at Leiden Academy Medical Center in The netherlands.
RR is a neurologist specialized in Huntington's Disease and Head of the department of neurology at Leiden University Medical Eye in The Netherlands.
Competing interests
The authors declare that they take no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study has been approved by the Medical Ethics Review Committee of the Leiden Academy Medical Heart in Leiden, The Netherlands (CCMO #NL 48029.058.fourteen, METC # P14.038). All eligible patients and their family-members were informed (both written and verbal) almost the purpose of the study, the expected elapsing and procedure, the right to refuse to participate and to withdraw from the research at any given time in one case participation has begun without whatever consequences. Written informed consent was obtained from all participants who were enrolled in the study.
Writer information
Affiliations
Corresponding author
Rights and permissions
Open Admission This article is distributed under the terms of the Artistic Eatables Attribution four.0 International License (http://creativecommons.org/licenses/by/four.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you lot give appropriate credit to the original writer(south) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Artistic Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zilch/1.0/) applies to the information made available in this article, unless otherwise stated.
Reprints and Permissions
About this article
Cite this commodity
van Bruggen-Rufi, M., Vink, A., Achterberg, W. et al. Music therapy in Huntington's affliction: a protocol for a multi-center randomized controlled trial. BMC Psychol 4, 38 (2016). https://doi.org/10.1186/s40359-016-0146-z
-
Received:
-
Accustomed:
-
Published:
-
DOI : https://doi.org/ten.1186/s40359-016-0146-z
Keywords
- Music therapy
- Huntington'southward disease
- Communicative and expressive skills
- Behavioral problems
- Quality of life
- Randomized controlled trial
Source: https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-016-0146-z
0 Response to "The Ffect of Music Gtherapy for Patients With Huntingtons Disease a Systematic Literature Review"
Post a Comment